
Hydrozid® is applied to a lesion directly from the canister. Hydrozid® does not require any preparation time; no foam tipped applicators, tubes or replacing of cartridges.


Hydrozid® is non-flammable, non-oxidizing and non-toxic. Hydrozid® does not require separate storage facilities or ventilated rooms. No safe precautions or protective equipment as such as gloves or googles are required.

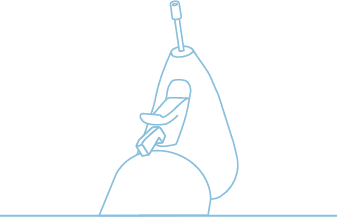
Remove Hydrozid® from the pack. Hydrozid® is locked (the disk extension is placed to the left). This feature prevents unintended spraying both while carrying Hydrozid® or between treatments.
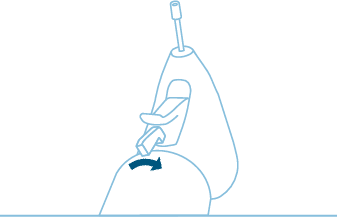
Move the disk extension to the right to open the spray head. Hydrozid® is applied to a lesion directly from the canister. No anaesthesia prior to treatment is required.
Hydrozid® is now ready to use. To avoid damaging the surrounding tissue use one of the application templates provided in the Hydrozid® pack.
Select the hole matching the size of the individual lesion. Freeze the lesion by applying Hydrozid® from a distance of 2 to 3 cm followed by a complete thaw. After a short interval, repeat the freeze-thaw cycle.
Several repeated freeze-thaw cycles are recommended as in a single treatment. The total duration of application to a lesion must be kept within the recommended maximum total (see panel).
For large lesions, it is recommended to apply the jet in circle movements from the center of the lesion to the external in a circle within the given area.
Acrochordon (skin tag)
2×3 to 2×6 seconds
6 to 12 seconds

Acrochordons, also called skin tags, are small benign fibroepithelial tumors that usually attach to the skin through a thin, raised stalk, often with a visible blood vessel, known as a peduncle.1 Skin tags may also be ”sessile”, i.e. fixed to the skin without a stalk.2
Skin tags are made up of collagen and emerge when extra cells grow in the top layers of the skin. Skin tags develop slowly over time when the skin is exposed to friction, such as between skin folds, in the axillae, on the eyelids, on the neck, below the chest, or in the groin.3
Skin tags vary in appearance from brownish to skin-coloured, and in size from less than 2 mm to 5 cm in diameter.1 The surface may be smooth or irregular.4
Skin tags occur in 25-40% of the population, and the prevalence is higher in women and with increasing age.3 In addition, the prevalence is higher among obese people.2 Just as diabetes is also a predisposing factor.1,4
Some may experience itching or pain when skin tags get caught in jewelry or clothes, and trauma to the skin tag may cause bleeding due to increased vascularisation.1 Some patients may also experience skin tags as being cosmetically unsightly.1 The above complications are the most common reasons why people seek treatment.
1. Morgensen, M & Jensen, A. N. (2022): Akrochordon, skin tag. Localised 17.02.2023 on: https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/hud/tilstande-og-sygdomme/noduli-cyster-polypper/skin-tag/.
2. Luba, M. C. et. al (2003): Common benign skin tumors. Am Fam Physician 2003;67: 729-38.
3. Venning, V. & Alexander, P. (2019): Skin tags. Australasian College of Dermatologists. Localised 18.02.2023 on: https://www.dermcoll.edu.au/atoz/skin-tags/.
4. Hahler, B. (2006): An overview of dermatological conditions commonly associated with the obese patient. Ostomy Wound Manage 2006;52: 34-6, 38, 40.
Actinic Keratosis (Non-Facial and Facial)
2×4 to 2×5 seconds
8 to 10 seconds

Actinic keratosis, also called solar keratosis, is considered to be premalignant skin changes, primarily in the basal cell layer of the epidermis1.
Among the causes for this development is long-term exposure to sun throughout life, and about 80% of all actinic keratoses are found in sun-damaged skin areas2.
Actinic keratoses are often located on the head, scalp, ears, and neck, on the back of your hand and the back of upper and lower extremities3,1. Actinic keratoses manifest as small, adherent pink and yellowish-brown scales. They vary in thickness from atrophic to hypertrophic, and in size from 1mm to several centimetres1.
In clinical terms, actinic keratoses are divided into three severity grades1,4.
Early-stage actinic keratoses may itch slightly. When the lesions become hyperkeratotic, they may cause both functional and cosmetic impairment2, and patients often seek treatment.
Until recently, it was assumed that grade III actinic keratoses were more dysplastic than grade II actinic keratoses. However, recent research indicates that both grades of actinic keratoses have the same level of dysplasia, which emphasizes that all actinic keratoses should be treated, irrespective of their thickness5.
If left untreated, actinic keratoses can penetrate the dermis, allowing the premalignant state to develop into non-melanoma skin cancer in the form of basal cell carcinoma (BCC) and particularly squamous cell carcinoma (SCC) of the skin4. However, timely treatment with cryosurgery can prevent this development.
1. Lægehåndbogen [Doctor’s Handbook] at sundhed.dk. 2018. Aktinisk keratose. Localised 25.01.2023 on: https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/hud/tilstande-og-sygdomme/skaellende-hudlidelser/aktinisk-keratose/.
2. Hædersdal, M. et. al 2014. Guidelines vedrørende behandling af aktiniske keratoser Udarbejdet for Dansk Dermatologisk Selskab.
3. Eisen, D., B., et. al. 2021. Guidelines of care for the management of actinic keratosis. J AM ACAD DERMATOl. OCTOBER 2021.
4. Lorentzen, H. F. 2017. Behandling af aktiniske keratoser og almen praksis. Rationel Farmakoterapi 8, 2017.
5. Mikkelsen, C., S. et. Al. 2016. Aktiniske keratoser og fotodynamisk terapi – En opdatering. Månedsskrift for almen praksis juni/juli 2016.
Verruca Vulgaris (Common Warts)
4×6 to 6×6 seconds
24 to 36 seconds
Common warts, also known as verruca vulgaris, are superficial viral infections of the skin caused by human papilloma virus (HPV).
Common warts may vary in appearance, but frequently occur as multiple, hyperkeratotic cauliflower-like papules on the skin. They most often range from 1-10 mm in diameter.1 The surface of the common wart has small black dots, sometimes invisible to the naked eye, representing blood clots in the capillaries of the wart. These capillaries can contribute to the diagnosis of a common wart, as this clinical observation is not seen in differential diagnoses such as callosities or soft tissue sarcomas. In addition, the patient’s fingerprint will not be visible on the surface of a common wart as is typically the case for callous skin, for instance.2
Common warts occur in places where the skin has been exposed to abrasions or other microtrauma, as the virus is inoculated into the skin through the epithelial tissue and penetrates further down into the deeper epithelial layers.3 HPV is resistant and spreads through both direct and indirect contact, leaving a large proportion of everyday objects as reservoirs of infection. Particularly in case of periungual warts, located around nails and nail walls, there is an increased risk of spread to the patient’s lips, oral cavity and tongue if the patient is a nailbiter.4 In addition, visible common warts may be perceived as socially unacceptable, as described in several studies. The fear of passing on infection may result in social isolation for the common wart patient, thus potentially affecting the patient’s mental health.1,5 Due to their long incubation time of 1-6 months, it is beneficial to treat warts in order to better break the chain of infection and reduce the infection of others.
1. Sundhed.dk – Lægehåndbogen [Doctor’s Handbook]. Vorter på hænder og fødder. Available: Vorter på hænder og fødder – Lægehåndbogen at sundhed.dk [2019, 25-10-2021].
2. James, W. D. et al. (2020): Viral Diseases. In: Andrews’ Diseases of the Skin, 19, 362-420.
3. Sil, A. et al. (2020): Journal of Paediatrics and Child Health 56 (2020) 989–998.
4. Dansk dermatologisk Selskab (2008): Hudlægen informerer om Vorter. Dansk dermatologisk Selskab · 1. udgave.
5. Baker, G. E & Tyring, S. K. (1997): Therapeutic approaches to papillomavirus infections. Dermatol.Clin. 1997 Apr;15(2), pp. 331-340.
Condyloma Acuminatum
2×6 to 6×6 seconds
12 to 36 seconds
Condylomata acuminata, also known as genital warts, are benign warts located in the anogenital area.
In more than 90% of cases, the development of condylomas is caused by human papillomavirus (HPV) genotype 6 and 111,2 and is considered the most frequently occurring sexually transmitted disease, with a transmission rate of 60% between partners, in the Western world. The high infectivity of condylomas is due to the thin mucosal surface, which is more susceptible to infection3.
In women, condylomas are most frequently seen on the labia, at the urethra, on the mount of Venus, around the perineum, and anus. Condylomas can also grow inside the vagina itself, and for example, sit on the cervix1. The incidence among women is greatest among young women under the age of 245. In addition, there is an increased incidence of condylomas among smokers4,6. The cure rate is higher for women than for men1.
In uncircumcised men, condylomas are most frequently seen on the head of the penis, on the ring around the head of the penis, on the banjo string, and on the inside of the foreskin. In circumcised men, condylomas are most frequently seen on the shaft of the penis1. The incidence among men is greatest in the 25-29 age group1.
Condylomas are rarely found in women like men in the oral cavity and in the mucous membrane of the eye3.
The condylomas can appear individually, several next to each other, or as fused tumor-like elements. Most often, 5-15 elements are seen in the same area, with a diameter of 1-5 mm5. Condylomas vary in appearance and will appear moist on the mucous membrane with a “cauliflower-like” surface. On dry and possibly hairy skin, the warts, especially on teenagers and young adults, will appear firmer and keratinized3. The color of condylomas can vary from pink to salmon-colored and from white/grayish white, to various shades of brown (pigmented elements). Condylomas tend to be non-pigmented, but in some cases appear pigmented on the shaft of the penis in the groin, perineum, and in the perianal area1.
The condylomas can cause itching and in the case of larger condylomas, maceration, irritation, pain, and bleeding6. Treatment will remove the visible changes on the skin, but since condylomas are a subclinical infection, there may be a risk of recurrence after treatment4,6. The incubation period is between 3 weeks – 8 months. For the same reason, patients with condylomas should be treated as soon as possible to break the chain of infection and prevent other recipients of the infection.
1. European Course on HPV-associated pathology: guidelines for primary care physicians for the diagnosis and management of anogenital warts. Krogh G von, Lacey CJN, gross G, Barrasso R, Schneider A Sex Transm Inf 2000; 76:162–168.
2. Recommendations on the prevention, diagnosis, and treatment of sexually transmitted infections. SST 2015.
3. Eassa, B. In et. Eel. 2011. Intradermal injection of PPD as a novel approach of immunotherapy in anogenital warts in pregnant women. Dermatologic Therapy, vol 24, 2011, 137-143.
4. Condylomata – Odense local. Located on 11.01.2020 at: https://www.sundhed.dk/sundhedsfaglig/information-til-praksis/syddanmark/almen-praksis/patientforloeb/forloebsbeskrivelner/icpc-oversigt/x-kvindelige-koensorganger-inkl-mammae/ condylomas-odense-local/.
5. Patel H, Wagner M, Singhal P et al. Systematic review of the incidence and prevalence of genital warts. BMC Infectious Diseases 2013;13:39.
6. Lacey CJ, Woodhall SC, Wikstrom A et al. 2012 European guideline for the management of anogenital warts. J Eur Acad Dermatol Venereol 2013;27:e263-70.
Lentigo Solaris
2×3 seconds
6 seconds

Lentigo solaris also known as “lentigo senillis”, “liver spots” and “age spots”, are benign changes on the skin that include hyperplasia of the epidermis and increased pigmentation of the basal layer1.
The changes on the skin occur due to sun exposure, and thus appear on sun-exposed areas of the body, such as the face, backs of the hands, shoulders, and back1, 2. The changes can develop slowly over years, or occur suddenly.1, 2
Lentigo solaris varies in appearance, from light brown to dark or black spots on the skin, from oval to irregular, and in some cases nodular in the lesion or slightly scaly. They also vary in size, from a few millimeters to several centimeters in diameter. The changes often become darker and larger proportionally with age2, 3. Lentigo occurs on sun-exposed skin, and most frequently among light-skinned people,
The incidence of lentigo solaris is higher in fair-skinned people who have been exposed to a lot of sun2.
Children with the rare, inherited skin disease xeroderma pigmentosum develop lentigo solaris in the first months of life, even after minimal sun exposure4.
Lentigo solaris can be cosmetically disfiguring for some patients, which is why they seek treatment.
1. Schwartz RA, & Okulicz JF, & Jozwiak S. (2019): Lentigo. eMedicine, Medscape, last updated april 2019.
2. Sundhed.dk (2021): Lentigo solaris. Accessed on 01.02.2023 at: https://www.sundhed.dk/sundhedsfaglig/laegehandbogen/hud/tilstande-og-sygdomme/pigmenterede-laesioner/lentigo-solaris/.
3. Chan, B. (2014): Solar lentigo: Bob Chan. Dermatology Registrar, Auckland Hospital, Auckland, New Zealand, 2014.
4. Tsatsou, F. el al. (2012): Extrinsic aging. UV-mediated skin carcinogenesis. Dermato-Endocrinology. Volume 4, 2012. pp. 285-297
Molluscum contagiosum (water warts)
2×3 to 2×6 seconds
6 to 12 seconds

Molluscum contagiosum, also called water warts, is a viral infection caused by a DNA poxvirus manifesting in the skin.1,2 Molluscum contagiosum is one of the five most prevalent skin diseases worldwide.2
Transmitted by direct skin-to-skin contact,2 molluscum contagiosum develops slowly over weeks. As they grow, the mollusca develop a central dimple, also known as umbilication.1
Molluscum contagiosum presents as dome-shaped papules containing cheesy material, the molluscum body. The mollusca have a smooth surface and vary in appearance from pale red to skin-coloured and in size from 3-10 mm.1,2
Molluscum contagiosum is most prevalent in children (about 9 out of 10 cases) of all ages, sexually active persons and in immunosuppressed individuals 1,2. The prevalence is also higher among atopics1,2 and in countries with a warm climate.2
In children, the mollusca are typically located on the extremities, trunk and face, often in body creases. Sexually transmitted molluscum contagiosum is located in the lower abdomen and the genital region. In immunosuppressed individuals, molluscum contagiosum more frequently presents as large, multiple mollusca.1
The incubation period is estimated to be 2-8 weeks,2 which means that molluscum contagiosum should be treated to break the chain of infection and reduce the number of further infectees. In some persons, molluscum contagiosum may also cause itching, eczema and secondary bacterial infections.1,2 Some patients may also experience molluscum contagiosum as being cosmetically unsightly. The above complications are the most common reasons why people seek treatment.
1. Morgensen, M & Jensen, A. N. (2022): Molluscum contagiosum, vandvorter. Localized 03.03.2023 on:
Molluscum contagiosum, vandvorter – Lægehåndbogen på sundhed.dk
2. Lacarrubba, F. et. al. (2022): New Developing Treatments for Molluscum Contagiosum. Dermatol Ther (Heidelb) (2022) 12:2669–2678.
Seborrheic Keratosis
2×6 to 3×6 seconds
12 to 18 seconds

Seborrheic keratosis, also called “seborrheic wart”, “senile wart”, “senile keratosis”, “brown wart”, or “wisdom wart” develops into an epidermal wart because of a benign proliferation of the surface epithelium1.
The cause of this development is still unknown but is frequently occurring and increases with age1. The prevalence is greater among people with lighter skin tones but is equally distributed among men and women2.
Seborrheic warts vary in appearance and may resemble a flat raisin, from skin-colored to brown-black, and between a few millimeters and 3 cm in diameter. Larger elements may also occur. They are most frequently located on the trunk but are also seen on the scalp, face, and extremities1.
Seborrheic warts are often asymptomatic, but can sometimes, due to bothersome itching or for cosmetic reasons, be the reason why patients seek treatment1.
Seborrheic warts do not have malignant potential and can be easily removed1.
1. Agner, T. & Jensen, A. N. (2022): Seborrheic warts. Available on 01.03.2023 at: https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/hud/tilstande-og-sygdomme/pigmenterede-laesioner/seboroiske-vorter/.
2. Thai, K. E. & Sinclair, R. D. (1999): Cryosurgery of benign skin lesions. Australasian Journal of Dermatology, 1999, 40, pp: 175-186.
Verruca Plana
6×3 seconds
18 seconds

Warts and verrucas are caused by a viral infection of the skin with a special variant of human papillomavirus (HPV).
Patients may perceive warts and verrucas as socially unacceptable if they occur in particularly visible places such as face or hands. This may result in social isolation affecting the patient’s mental health.
Verrucas on the sole of the foot are pressed flat during the daily mobilisation and grow inwards. As the verruca pushes into the sole of the foot, its hyperkeratotic, rough surface may be a source of pain that restricts mobilisation.
A shared feature of warts and verrucas is that the virus is highly resistant and spreads through both direct and indirect contact, leaving a large proportion of the population and everyday objects as reservoirs of HPV infection. Although HPV persists in the skin after treatment of the actual wart or verruca, treatment can prevent the spread of the infection.
As the incubation period is 1-6 months, warts and verrucas on your hands and feet should therefore be treated immediately to break the infection chain and reduce infection of others.1, 2
1. Baker GE, Tyring SK. Therapeutic approaches to papillomavirus infections. Dermatol.Clin. 1997 Apr;15(2), pp. 331-340
2. Kazeminejad A, Ghahari MJ, Hajheydari Z. Treatment of Warts in Children With Focus on Recalcitrant Warts: A Narrative Review. Journal of Pediatrics Review. 2020; 8(4):237-246
Verruca Plantaris
4×6 to 6×6 seconds
24 to 36 seconds

Warts and verrucas are caused by a viral infection of the skin with a special variant of human papillomavirus (HPV).
Patients may perceive warts and verrucas as socially unacceptable if they occur in particularly visible places such as face or hands. This may result in social isolation affecting the patient’s mental health.
Verrucas on the sole of the foot are pressed flat during the daily mobilisation and grow inwards. As the verruca pushes into the sole of the foot, its hyperkeratotic, rough surface may be a source of pain that restricts mobilisation.
A shared feature of warts and verrucas is that the virus is highly resistant and spreads through both direct and indirect contact, leaving a large proportion of the population and everyday objects as reservoirs of HPV infection. Although HPV persists in the skin after treatment of the actual wart or verruca, treatment can prevent the spread of the infection.
As the incubation period is 1-6 months, warts and verrucas on your hands and feet should therefore be treated immediately to break the infection chain and reduce infection of others.1, 2
1. Baker GE, Tyring SK. Therapeutic approaches to papillomavirus infections. Dermatol.Clin. 1997 Apr;15(2), pp. 331-340
2. Kazeminejad A, Ghahari MJ, Hajheydari Z. Treatment of Warts in Children With Focus on Recalcitrant Warts: A Narrative Review. Journal of Pediatrics Review. 2020; 8(4):237-246
Cervical Contact Bleeding
6x6 seconds
36 seconds
Cervical contact bleeding is bleeding that originates from the cervix. There are several potential causes for bleeding from the cervix, and women are usually encouraged to go to a gynecologist for evaluation if they experience cervical bleeding. Cervical bleeding after copulation or another contact with the cervix is relatively common and may result from a wide range of non-cancer-related pathologies, such as cervical polyps, various metaplastic states1, 2 ectopic/erosions3, and cervicitis.4
1. Michelle J. Khan and Karen K. Smith-McCune. Treatment of Cervical Precancers: Back to Basics. Obstet Gynecol. 2014 June ; 123(6): 1339–1343.
2. Mahira Jahic, Elmir Jahic, Mirsada Mulavdic, Azra Hadzimehmedovic. Difference Between Cryotherapy and Follow Up Low Grade Squamous Lesion of Cervix Uteri. MED ARCH. 2017 AUG; 71(4): 280-283
3. Mohanty KC, Rand RJ, Berry B. Cryotherapy in the management of cervical ectopy. Genitourin Med. 1985 Oct;61(5):335-7.
4. Ben-Haroush A, Yogev Y, Beckerman A, Levavi H, Kaplan B. A mobile aerolsol cryotherapy device (Histofreezer) for treatment of cervical contact bleeding: a pilot study. Jour Obs Gyn 2003; 23:177- 78.
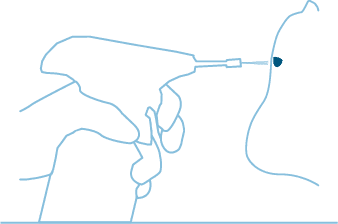
Gingival Melanin Hyperpigmentation
6x6 seconds
36 seconds
Gingival Melanin Pigmentation (GMP), which is benign however a cosmetic concern, is a focal pigmentation of endogenous origin that occurs because of the excessive deposition of melanin. The color of the oral melanin pigmentation may vary from light to dark brown or black, depending on the amount and localization in the tissue.1
1. Arikan F, Gürkan A. Cryosurgical treatment of gingival melanin pigmentation with tetrafluoroethane. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:452-7.
The Hydrozid® team is always here to support any inquiries you may have.
© 2024 Bibawo Medical A/S – Design by Aveo
We use cookies to optimize our website and our service.